Vaccines
Article curated by Rowena Fletcher-Wood
There are many unknowns and open questions surrounding vaccines – but they might not be the first questions that come to mind. Vaccine history tells the story of a long struggle with a small number of recurring myths that we have strong scientific evidence to dismiss. But there are still unknowns – and will be so long as our biological knowledge remains incomplete. So what are the myths, and what are the real mysteries?

Making Vaccines
What is the immune system?
The immune system is not a thing with edges like a lung; more, it’s a relationship, a complex network of organs, cells, tissues and glands that cooperate to identify and remove foreign cells that have snuck into the body by creating, releasing and educating antibodies.What is an "adjuvant" and why are they added to vaccines?
Adjuvants are immune system stimulants that kid the body into thinking there was a lot more of an infectious agent in a vaccine than there really was. They either concentrate the antigen providing a high density blob of it, or make the body produce lots of cytokines (which in theory create a bigger immune response, but this doesn’t always happen, so we’re not sure exactly how cytokines work). Aluminium salts are common adjuvants that have been safely used in vaccines for 60 years. They’re nothing unusual, and we encounter lots of aluminium salts entering our body in food or water.Learn more about Cytokines.


 3
3
Testing Vaccines
The process for testing vaccines is lengthy, and can take up to 10 years, involving computer modelling, animal testing and finally three rounds of testing in humans. Under normal circumstances, the testing occurs in 20-100 healthy human volunteers first (who must be made aware of the risks), followed by a larger sample of at-risk people facing the disease. During this second step, the dosage is assessed, placebos are used alongside the real vaccine and any side effects are identified and studied. Side effects can be tricky to separate from normal ups and downs without the use of placebo.
Learn more about Placebo.

 2
2
Occasionally, active and devastating diseases force trials to skip to this second phase – like the recent Ebola crisis, where Africans who had come into contact with the sick were offered a potential vaccination. The last stage of trials involve large numbers (at least thousands) of volunteers from diverse backgrounds. Monitoring continues even after a vaccine has been approved – after all, there is still a risk. We can’t know if a drug is safe until after we have done the tests, though we can minimise risk.


Using Vaccines
Sometimes, it may be desirable to give a vaccine for a purpose other than the one it was originally designed for.
Should we give HPV vaccines to boys?
Currently, girls in the UK are vaccinated against the Human Papilloma Virus (HPV), a sexually transmitted disease which can lead to cervical cancers. They are given the vaccination around age 12, before they become sexually active, because it doesn’t work for women who have already been infected by HPV. Although we don’t know if this vaccine works, rates of genital warts are going down, which can be HPV-related. Meanwhile, although boys don’t have cervixes, some want them to be vaccinated too – reducing the spread of the disease and protecting them against head and neck cancers that can be linked through oral sex to HPV. Others say it’s not worth vaccinating boys – vaccinating girls will be enough to eliminate HPV in just 20 years, giving them herd immunity.

Eight real risks of vaccination
Risk 1. Probably the main risk from vaccinations is Syncope - people fainting and then falling and hurting themselves. Fainting is a common reaction to a lot of medical procedures (which is why they make you sit down), especially vaccination, although we don’t know why. It’s unlikely to be due to ingredients because these vary between vaccines, but some vaccines do have higher faint-rates than others. We also don’t know why teenagers faint more than children or adults (62% of fainters are teenagers)[1].



Risk 2. As long as live strains of virus are being used for vaccines, there’s a risk of reversion to pathogenicity. This is where disabled, safe strains mutate back to dangerous ones that put unvaccinated people at risk.


Viruses are ever-adapting, especially when living in a host In one case of a man with immune deficiency, mutated, paralysis-causing forms of polio were discovered inhabiting his gut. He’d been vaccinated as a child before his condition was known, and carried the virus ever since. Because of the live virus in the oral polio vaccine, children “shed” the disease when they toilet for a few weeks after they’re given it – this man had been doing that with a more dangerous strand for years. Because of the risk of pathogenicity, in 2004, the UK switched to a less potent, but less risky inactivated polio vaccine which is injected. Another way to overcome the risk is to just use fragments or subunits of a virus, but this isn’t always possible.
Learn more about Virus Evolution.


 2
2Risk 3. One option for creating new, safe vaccines is genetically engineering them. However, professionals are unsure whether we have sufficient genetic knowledge to genetically engineer effective vaccines or whether, if we did, we could ensure they couldn’t either revert to pathogenicity, or combine with other viruses/bacteria to produce new diseases.


 2
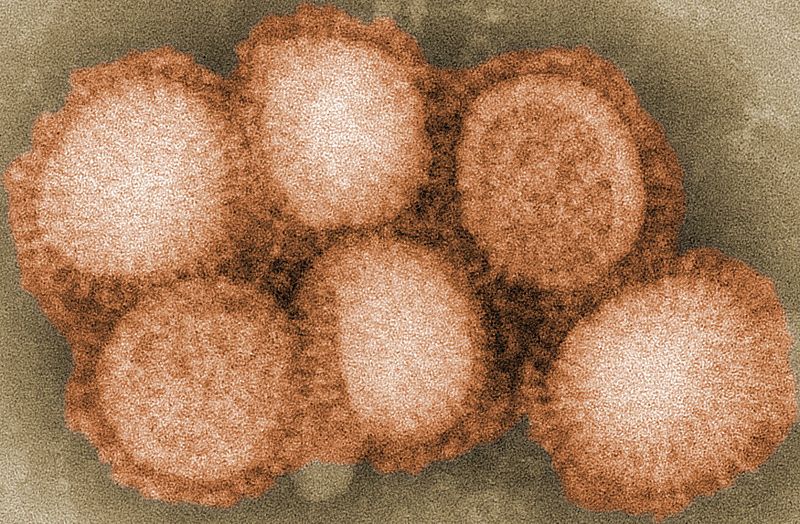
2Risk 4. As well as mutating to become dangerous, already dangerous diseases might adapt to become unrecognisable by our immune systems by changing their epitopes, or molecular shapes. Vaccines normally work by pretending to be a virus or bacterium that the body then fights off and learns to fight off next time. This is why one disease can provide immunity against another (like cow pox and smallpox) – they have similar epitopes, and get bound to and fought off the same way. But when a virus changes its epitope enough, like with seasonal influenza, the body doesn’t recognise how to kill it, and vaccinated people are suddenly at risk. Although this isn’t a direct risk of vaccination, vaccination makes people less careful and could exacerbate incidences. This is why disease elimination is important.


 3
3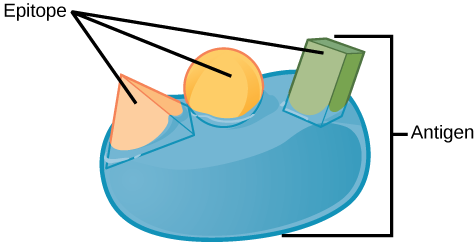
Risk 5. Vaccines can cause our body to attack itself. In 1885, Louis Pasteur produced the first inactivated rabies vaccine by drying rabbit brains and treating them with formalin. The people he gave it to developed rabies immunity, but some also developed a fatal autoimmune disease. Overwhelmed by large numbers of rabbit central nervous system molecules, their immune systems became unable to distinguish “self” from “non-self” molecules, and turned to destroying their own cells.
Whilst the killed vaccines we use today contain much less rabbit (if any) and are usually heat or chemical killed, a small risk remains for susceptible individuals and, as a compromise, vaccines are often less successful.
Learn more about causes of autoimmune disease.


 3
3
Current work at the University of Oxford has focussed on T cells, cells that already exist naturally in your body to fight autoimmune disease and transplant rejection. T cells are biological messengers that regulate the immune system and tell it when to and when not to turn on its defences. Researchers think these could be extracted, grown in petri dishes and put back in your body to to mediate your immune response to autoimmune diseases and the presence of new organs. This bypasses the dangers of a suppressed immune system after autoimmune disease or as a result of taking immunosuppressants to force the body to accept an alien organ. People with transplants and autoimmune diseases would not need to rely on herd immunity and their immune systems could remember previous vaccinations and keep on the alert for new invading pathogens. The same cells could also be used to treat autoimmune disease. Clinical trials on T cells are now underway.


 2
2Risk 6. Sometimes vaccines are given therapeutically to already infected individuals with the hope of rousing their immune system to help them fight the disease off. Therapeutic vaccination is being tested with HIV patients[2].
One kind of therapeutic vaccination is passive immunisation, where antibodies from the immune are injected into the unwell. This can alleviate symptoms, but also lowers the need to make your own antibodies, so our unwell person might become more susceptible to the disease and not develop immunity at all. Passive immunisation is usually only used for tetanus, diphtheria or botulism, where exotoxins are produced that kill rapidly if not fought off early on.


 2
2Risk 7. Making and studying vaccines means keeping viruses, which poses a risk to the handlers. Although this risk is carefully managed, things can go wrong, such as in 1978, when clumsy handling of a smallpox virus in the University of Birmingham led to the death of a medical photographer and, as a result, the suicide of the head of department[3].
Risk 8. We don’t know if live virus vaccines can harm babies, and as such don’t recommend them (such as MMR, HPV and chicken pox) during pregnancy. However, some non-live vaccines are safe and can protect babies, who only have antibodies from their mothers for a few months after birth.

Vaccinating a breastfeeding mother is also safe – breast milk doesn’t simply leak out whatever’s in your body, but changes its formula in response to what your baby needs. Scientists think this could be a direct response to a baby’s physical health, due to “backwash” – the baby’s saliva entering the breast to signal which antibodies it needs her to make.


Side effects of vaccines
There are three kinds of side effects to vaccines: injection site reactions, caused by the needle penetrating the skin, immune system reactions, where we feel the effects of the vaccine working to teach the immune system to fight off the disease, and, most seriously, allergic reactions - Immune system overreactions to harmless foreign agents that result in very serious unwellness and can be life-threatening.
Side effect 1. Injection site reactions, such as pain, swelling or redness, are caused by damaged tissue (or a local allergic reaction). At worst, extravasation – a bit of the drug leaking out from the blood vessel – can cause bad blistering and skin damage that might even require plastic surgery to fix up.
Side effect 2. Immune system reactions mostly involve feeling unwell. This unwell feeling doesn’t mean you have the disease, but it means your body recognises there is something “bad” inside you and is dealing with it. The unwell feeling is caused not by the virus, but your own immune system - you can see this when you get physical stress reactions, like rashes and inflammation where there are no microbes involved of any kind. The immune system does various things to help clear an infection: swelling up an area to wall off an infection, coughing, sneezing, vomiting and diarrhoea to eject unfriendly microbes, and feeling lousy to make you sit still and keep warm. Not getting side effects doesn’t mean your immune system isn’t working – just that it’s less worried about the situation. Side effects differ person to person, vaccine to vaccine, and time to time. We don’t know why these variations occur, and can’t predict them. However, lists of common side effects can help us make guesses.
Febrile seizures can be one rather scary side effect of vaccines. We don’t know what causes febrile seizures, but they happen to 1 in 25 children between 6 months and 3 years old, mostly when they have a fever and temperature of 39°C or more. During a febrile seizure, the child loses consciousness, spasms and goes stiff. It normally lasts for 1-2 minutes, and has no lasting side effects. Some children will experience several, and whilst some may be brought on by the first MMR vaccination, others are prevented by vaccinating children against diseases that cause fevers.



Side effect 3. Allergic reactions happen when the immune system overreacts to harmless things like pollen. Allergic reactions include hives, skin irritations, swelling, low blood pressure and anaphylactic shock, which can be dramatic and potentially life-threatening. Most compounds that may be present in vaccines that cause allergic reactions are food-based, such as egg. Some viruses are grown and developed in eggs, and so traces of egg can sometimes be found in tiny amounts in vaccines.
Other additives include stabilisers to protect vaccines during freeze drying, such as sugars, amino acids, proteins including gelatine, or preservatives added to prevent the growth of bacteria or fungi. Antibiotics may be found in some vaccines to help prevent bacterial contamination whilst they’re growing in the eggs – although the antibiotics responsible for most allergic responses (penicillins, cephalosporins and sulfa drugs) are not used. A high standard is set for vaccine purity because they are given to healthy people.
We think that allergies turn up because the body isn’t well calibrated to detect “really bad stuff” from “okay stuff” – we have so little disease that it overreacts to harmless allergens! Less developed countries where disease rates are high see fewer allergies. Which would kind of mean that vaccines cause allergies... but only because they’re so successful at what they do.


 2
2Why would a vaccine, or certain batches of a vaccine, be withdrawn or recalled?
Vaccines are usually recalled because we don’t know if there’s a problem or not – as a precautionary measure. Most are recalled voluntarily by the manufacturer because of small irregularites during the trials (usually inconsistent effectiveness), and you don’t need to do anything if you're already vaccinated with these. Very few are recalled because of reports of adverse effects, although some are recalled because they’re not effective enough – which means you may need to get re-vaccinated.On a very few occasions, vaccines have had notably bad effects, such as the Cutter Laboratories polio vaccine of 1955, which caused 250 cases of polio and left many people paralysed. More recently, the 2009 GlaxoSmithKline Pandemrix vaccine against swine flu was found to cause narcolepsy in a small number of individuals – a permanent condition where people fall asleep uncontrollably, even in the middle of doing something. In these cases, narcolepsy was caused by the deletion of 70,000 brain neurons that made the hypocretin hormone that keeps us alert.
It’s thought that the swine flu vaccine of 1976 caused Guillain Barre Syndrome in 1 in 100,000 people – although scientists still don’t know why. Guillain Barre Syndrome is a life-threatening neurological disorder that causes limb weakness. It is more often caused by flu than the flu vaccine. There were also reports of Guillain Barre Syndrome which may or may not have been related to a meningitis vaccination in 2005 with Menactra. The FDA and CDC were
not able to determine if any or all of the cases were due to vaccination. While the CDC recommendation for routine vaccination did not change in general terms, they did note that
the timing of onset of neurologic symptoms within 1--5 weeks of vaccination among reported cases continues to be of concernand recommended
that persons with a history of GBS not receive MCV4.


Disease Elimination
Why isn’t there a vaccine for all diseases?
Some diseases, like sickle cell anaemia, are genetic, so you can only be infected if your parents are sufferers or carriers. Vaccines only work against diseases spread by external vehicles, because these involve foreign agents entering the body which can be identified as intruders and sent packing. This also explains why we can’t vaccinate against cancer. Although we can vaccinate against some of the viral infections that can bring on cancer (like HPV), cancerous cells are our own, and they look like our own. The immune system therefore doesn’t attack them and kill them, and if it did, how would it know where to stop? – It might wind up destroying other very important cells in the body.

 2
2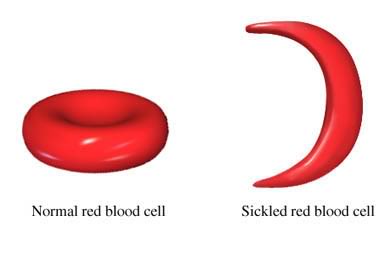
Some diseases can also effect your immune response to other diseases. In the 1960s, the introduction of the measles vaccines led to a drop in the number of cases of a measles - but it also led to a rapid decrease in all infectious diseases in children at a rate that cannot be explained by general improvements to healthcare and sanitation. In some developing countries, this has meant an 80% drop in the mortality rate. Although they’re not sure, scientists now think they have the answer: "immune amnesia", the phenomenon by which having measles not only temporarily suppresses your immune system, but also erases it’s log book - making you susceptible again to diseases you once defeated. Computer modelling epidemiological data from the from Europe and the states showed that numbers of measles cases pre-vaccine were an excellent statistical predictor of the number of deaths from other infections two or three years later. So that’s one jab to have.


 2
2However, even amongst non-genetic diseases, we can’t vaccinate for everything. Some, like the common cold, mutate rapidly and turn up looking different each time. Our bodies don’t recognise these new versions, and we don’t know how to create a vaccine that might help them to. There are too many versions of the cold mutating too quickly to develop vaccines against them all. Some diseases just exist in too many versions, such as salmonella, which has over 2200 serotypes - categories of organisms, microorganisms or cells within one species that are distinguished by characteristics such as surface proteins for bacteria.


Similarly, there is no vaccine against HIV. HIV contains a faulty enzyme that helps it change quickly – mutating 1 in every 2000 nucleotides, so every individual carries different kinds in different organs. This makes the disease hard to fight with drugs as well as awkward to vaccinate against. It also makes it hard to recognise an immune response against HIV, made worse by the fact the disease harms us by destroying our immune systems. However, because 90% of AIDS-related deaths happen in poor countries, it’s impossible to disentangle social limitations such as infrastructure and cost effectiveness from biomedical challenges.


 2
2Not all diseases need to mutate to deceive the immune system. Some have evolved decoy proteins that slow down the immune system, distract the immune system into attacking the wrong things or disguise a pathogen as a harmless self cells. Again, it’s hard to tell what a good immune response against these diseases would be, and as such we haven’t been able to design them.


 3
3
Other times, we may not have an immune response against a disease at all, or a very feeble one. For example, we have pretty much no idea how the immune system could destroy syphilis (because it doesn’t). It’s a global and ancient disease, easily killed with antibiotics, but not by the immune system. We can catch it again and again. That doesn’t mean the body doesn’t try – a positive test for syphilis is actually the test for syphilis antibodies – and these antibodies aren’t totally ineffective, because having syphilis once does means you develop a resistance against catching it again. But you can still get it. Syphilis antibodies stay in your bloodstream for a while (meaning you continue to “test positive for syphilis”), but they can eventually fade away, so it’s possible this only provokes a “short-term” immune response[4]. Theories suggest it’s a “stealth pathogen”, hiding behind unreadable, frequently changing proteins to incubate and spread[5]. It’s also a multi-stage disease, which may be why it's so tough[6].


Why isn't 100% vaccination 100% effective?
Provoking an immune response isn’t always enough to develop immunity. In a population of 100% vaccinated people, about 5% could still get a disease, although when they do, it’s often milder, such as in the case of chicken pox. Unvaccinated children with chicken pox have a rash, fever, brain swelling and pneumonia, whilst vaccinated children are usually only subject to the rash and a temperature. In the UK, the majority of people are vaccinated, so vaccinated people vastly outnumber unvaccinated people. As such, the vaccinated people who get a disease slightly outnumber unvaccinated people who get it, just because of statistics. This does not mean that vaccinated people are more likely to catch the disease!Although vaccines provoke immune responses, there are various different kinds of immune response. The immune system’s first job is to recognise pathogens as “non self” (antigenicity), then kill them (immunogenicity). A vaccine is usually injected and quickly ends up in the blood. However, when an infectious agent gets into the body, it may be through the nose, mouth or skin, and go to different bits of the body, where there are different antigens. These antigens may not know how to kill the non-self cells, or do it more slowly. Some people may just not fight off a disease quickly enough: we all have higher or lower sensitivities to infectious agents, and will respond to higher or lower loadings. This is why we need “herd immunity” - enough vaccinated people to shelter the unlucky ones.
Why can vaccines wear off?
Some diseases are remembered by the immune system, whilst other ones get forgotten. Live attenuated vaccines usually produce stronger immune responses than deactivated ones, and so the body “remembers” the disease better, and longer. After suffering from cholera, the body remembers the disease and develops long-lasting immunity, but the kind of cholera you get will affect the strength of that immunity. So far, the vaccines developed to combat cholera have been unable to produce the same results.Recently, researchers discovered that there really is a long- and short-term memory where the immune system is concerned, depending on which kinds of cells fight the disease. Ensuring we trigger long rather than short term memory is now the key challenge in vaccine design. This could be important not only for longer lasting immunity, but also for safeguarding against the rebound effect, where bouts of disease may be triggered by people who have had a temporary vaccination being less disease conscious and aware.


 3
3Why can you catch some diseases again?
Seasonal influenza viruses evolve continuously, which means that people can get infected multiple times throughout their lives. So is there a point in the flu vaccine?Flu is not just a bad case of the common cold – as well as cold-like symptoms it includes muscle aches, fever and headaches and can kill, especially amongst the old, young, or immune-compromised. Every now and then, flu pandemics arrive, when an unrecognised strand suddenly infects large numbers of people (some severely and some more mildly, although we don’t know why). The vaccine is mainly aimed at preventing huge numbers of deaths in these pandemics, and guards against new strands such as zoonotic avian or swine flus.
100% vaccination is not always 100% effective where disease is harboured by species other than humans. Several very nasty diseases that devastate human populations do their mutating and spreading in plant and animal hosts (such as badgers), only moving across when we come into contact with them. By the time we do, they no longer look like the versions we developed vaccinations against, and so keep rearing their ugly heads. These diseases are called zoonoses, and include tuberculosis, yellow fever and Ebola. It’s simply too hard to capture and vaccinate enough animal reservoirs, and so at present we don’t know how to eliminate these diseases.
Humans can also be carriers of some diseases, they're not affected themselves and so spread it about; such as typhoid, where only 2-5% of people see symptoms; or tuberculosis, where experts think a third of the world’s population is harbouring the latent virus.


 2
2


 2
2
Importantly, around 1 in 4 people who had chicken pox as a child develop shingles later on. Shingles is like chicken pox, but it’s not the same. It happens when the hibernating chicken pox virus is reawakened for reasons that aren’t entirely clear. It may be because of age related immune senescence, since the chance of getting shingles increases with age. Shingles lasts longer than chicken pox and is occasionally fatal (1/1000 cases in the over 70s)[10]. The shingles blister contains the chicken pox virus and can cause chicken pox, but you can’t catch shingles from people with chicken pox. We don’t know yet whether the chicken pox vaccine would reduce the chance of getting shingles, increase it, or have no effect on it. The chicken pox virus isn’t administered as a standard in many countries, including the UK. This is because the a vaccination programme would probably increase the number of cases of shingles and adult chicken pox for the first 100 or so years[11]. They’d be more cases of shingles because, with less chicken pox about, adults with natural immunity would encounter the disease less, and receive fewer immune boosts. They’d be more cases of adult chicken pox because, with less chicken pox about, more unvaccinated children wouldn’t catch it until they’re grown up - and the disease is more serious. This also means it would take a long time for the vaccine to become cost effective, as lots more people would be more ill in the short term. However, these problems wouldn’t last. Eventually, enough people would be vaccinated to create herd immunity.


 3
3Why are we “storing” some vaccines/diseases?
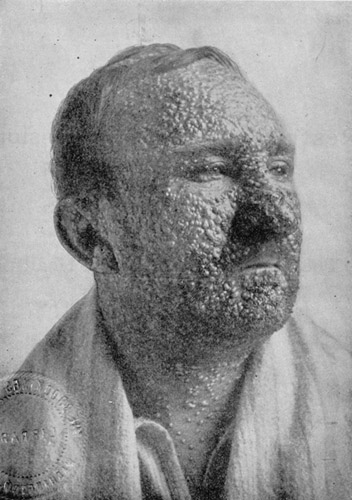
100% vaccination is only effective so long as vaccination programmes go on. For example, we stopped vaccinating people against smallpox 20 years ago when the disease was declared eradicated. However, stores of easily spreadable or devastating diseases including smallpox, polio and anthrax are kept and maintained in various scientific laboratories. Originally, smallpox was kept for scientific research with the expectation it would be destroyed, but now suggestions that it could be used for bioterrorism (or in the case of polio, that it could re-emerge) mean that people are keen to hold onto it in case a vaccine is ever required. Arguably, if we’d never stored it, that risk would never exist. The smallpox vaccine is not a friendly one, killing 1-3 people per million doses during the 1960s[12]. Although a weakened version, the smallpox virus caused widespread devastation around the globe, killing 10% of Europeans in the 18th century, and massacring the population of Mexico, which dropped from 25 million to 1.6 million between 1518 and 1620; and it has been cited as instrumental in the fall of the Aztec and Incan empires[13].

Myths
Myth 1. SIDS (Sudden Infant Death Syndrome) and vaccines are connected.
Vaccines tend to be given to babies around the time when they are most likely to suffer from SIDS. There is no statistical correlation between the number or timing of vaccines and SIDS, and no studies have found any link[14]. Meanwhile, SIDS deaths have declined since it was recommended to sleep babies on their backs[15].


Myth 2. Vaccines can overload your immune system.
We are exposed to innumerable foreign agents every just by eating, touching and sensing things, many of which are in some way harmful to us. We rarely notice and our body overwhelms most of them and flushes them back out. Although we have more vaccinations now than ever before, modern vaccines use far less microbe ingredients because they are better designed and include only the bits we need to include. Today vaccines contain less than 10% of the pathogens they did in 1980, a miniscule amount compared with our everyday encounters. According to CDC Atlanta, simultaneous vaccination with multiple vaccines has no adverse effect on the normal childhood immune system
. In fact, the opposite may be true, we may not encounter enough infectious agents, and may be getting allergies as a result.
Maybe what we need is parasites (seriously, this is something doctors are wondering about).

 2
2
Myth 3. Vaccines can give you mad cow disease.
This has never happened. Some vaccines use bovine-derived materials, which may be an issue for people with allergies or certain religious or dietary alignments. However, pharmaceutical ingredients are subject to tight regulations and since ensuring it contains the right amounts of the right kinds of pathogens is its purpose, the presence of other diseases is extremely unlikely[16].


Myth 4. Formaldehyde in vaccines causes cancer.
Formaldehyde is used during vaccine production and may be present in trace amounts. High concentrations of formaldehyde cause cancer when inhaled through the nose, but the quantities found in vaccines and injected into the blood stream are much smaller than the amount produced by your body during normal metabolism, in processes such as building the essential amino acids that we need to live.


 2
2Myth 5. Vaccines cause autism
In 1998, Andrew Wakefield and 12 other authors published a paper claiming that autism, a developmental disorder that can take the form of a communications disability, and gastrointestinal disorders were caused by the combined MMR vaccine, claiming that vaccination should occur for these diseases, but separately. The study was based on examining just 12 specially selected children. Vaccine trials normally start with 20-100 volunteers, then move on to hundreds and finally thousands in a three step expansion process. Twelve just isn’t enough people for a fair study. Since vaccine overload is not a thing, there is no scientific reason why combining vaccines should have a negative effect.
Andrew Wakefield was later struck from the medical register following the retraction of the paper by ten of his co-authors, the revelation that he had conflicts of interest (investment in rival non-combined vaccines for these diseases) and allegations of both data falsification and unethical, invasive examinations of children. Many studies have since proven no link between MMR vaccination and autism, or indeed, any vaccination and autism[17][18][19].
Thimerosal is an adjuvant in vaccines that has been accused of causing autism or other illnesses. Thimerosal is a preservative containing 50% mercury (a potent neurotoxin) by weight and used in some vaccines. The mercury in thimerosal is ethylmercury. After warnings of the harmful effects of methylmercury in fish, the public exerted pressure to have thimerosal in vaccines reduced to trace amounts. However, whilst methylmercury can build up in the body until it reaches toxic levels, ethylmercury is readily broken down and removed, so it doesn’t build up to harmful levels. Many studies have looked at and failed to find any link between thiomerosal and autism, or any other disease[20][21][22][23].
Learn more about Autism.


 3
3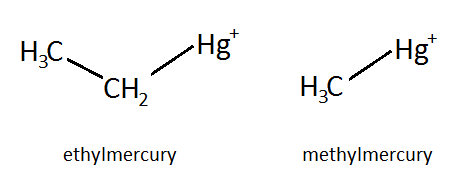
Coronavirus vaccine
Vaccine hesitants may be surprised, but ‘flu vaccine recipients from last season have been shown to be much less likely to contract COVID-19, and much less likely to suffer complications, or likely to suffer few complications, if they do. This is in contrast to the fear that it might cause coronavirus (no evidence) or make you more vulnerable (now disproven). The study looked at 27,000 people in March-July 2020, and variables including ethnicity, race, gender, age, BMI, smoking status and comorbidity were controlled for[24]. We don’t know why this works, but it remains an interesting finding! Longitudinal studies have been born off the back of it.


 2
2
Researchers have found the SARS-CoV-2 coronavirus mimics host RNA to “silence” distress calls by using certain proteins. Coronavirus uses “nsp14”, a protein key for virus reproduction. They are looking into how to “interfere with” this protein to bypass the silencing system, and have been able to shut it off in some cases, helping the body find and fight the virus sooner[25]. They used computer simulations to do so, along with biochemical characterisation.


 3
3Vaccines of the Future
Vaccines may have been around for a while, but there’s still lots we don’t know about them, and many possible ways of making them better. One challenge is prions – pathogens with the same primary amino acid structure as our own proteins (some say vaccines can’t be made against the prion, but can they?). They look like self molecules, but they don’t behave like them.


 2
2Another challenge is DNA vaccines – the idea of inserting DNA into the muscle without a carrier protein for the body to recognise or to replicate it. However, we think it will work (and have had some success in animals) with the right ‘promoter’ that can get it into our own cells to replicate there. One method puts the DNA on gold particles and shoots them into the body using a gas-pressurised gun.
We’re already experimenting with conjugate vaccines, which use bits (subunits) of pathogens bound up with bacterial proteins known to stimulate a massive immune response. These first started appearing in the 1990s, and are now used for meningitis C and some flu vaccines. However, new research is looking at genetically engineering subunits or non-pathogenic infectious agents. This kind of genetic engineering could also take place in plants, using genetics to code for the production of conjugate vaccines so that when you eat them you get vaccinated. We don’t know if it would work, but this could potentially solve the logistic problems of vaccinating people who require multiple doses in developing countries. However, it remains challenging; as we don’t normally exhibit immune responses against food, if we could provoke one how would that impact the rest of our diet and our normal reactions to infectious agents?


 3
3
More recently, scientists and researchers have predicted a new paradigm shift from biological to chemical vaccines. There are several problems with biological vaccines that chemical vaccines might be able to overcome. They need to be cultured in carefully controlled laboratory conditions, isolated and purified and even then often stimulate poor immune responses – hence the need for conjugate vaccines and immune response stimulating coatings. Now new companies are working on developing well-defined synthetic, chemical vaccines by designing artificial carbohydrates made by gluing together monosaccharide building blocks. These chemical alternatives will be more stable, voiding the need for special transport conditions such as refrigeration and growth media like egg, faster and cheaper to make, and easier to prepare in bulk. What they won’t address is the conundrum that creating a vaccine that stimulates an immune response still doesn’t guarantee protection. However, it might make the development of more vaccines easier – only 27 pathogens have functional vaccines in use today. One start-up company, Vaxxilon, have got as far as building a semi-synthetic vaccine against pneumococcus made from a biological protein and synthetic carbohydrate. Full synthetic alternatives are planned.


 2
2This article was written by the Things We Don’t Know editorial team, with contributions from Ellen Moran, Ginny Smith, Johanna Blee, and Rowena Fletcher-Wood.
This article was first published on 2016-12-21 and was last updated on 2021-04-14.
References
why don’t all references have links?
[1] Centers for Disease Control and Prevention. "Syncope after vaccination--United States, January 2005-July 2007." MMWR. Morbidity and mortality weekly report 57.17 (2008): 457
[2] Macatangay, B,J,C., et al., (2016) Therapeutic Vaccination With Dendritic Cells Loaded With Autologous HIV Type 1–Infected Apoptotic Cells Journal of Infectious Diseases 213(9):1400-1409 DOI: 10.1093/infdis/jiv582
[3] Barquet, N., (1997) Smallpox: The Triumph over the Most Terrible of the Ministers of Death Annals of Internal Medicine 127(8_Part:635- DOI: 10.7326/0003-4819-127-8_Part_1-199710150-00010
[4] Sparling, P. F., Elkins, C., Wyrick, P. B., & Cohen, M. S. (1994). Vaccines for bacterial sexually transmitted infections: a realistic goal?. Proceedings of the National Academy of Sciences, 91(7), 2456-2463.
[5] Peeling, R,W., Hook, E,W., (2006) The pathogenesis of syphilis: the Great Mimicker, revisited The Journal of Pathology 208(2):224-232 DOI: 10.1002/path.1903
[6] Cameron, C,E., Lukehart, S,A., (2014) Current status of syphilis vaccine development: Need, challenges, prospects Vaccine 32(14):1602-1609 DOI: 10.1016/j.vaccine.2013.09.053
[7] Why doesn't the UK have a chickenpox vaccination programme - the geek father blog
[8] Shapiro, E,D., et al., (2011) Effectiveness of 2 Doses of Varicella Vaccine in Children Journal of Infectious Diseases 203(3):312-315 DOI: 10.1093/infdis/jiq052
[9] Varicella UK government Green Book
[10] Van Hoek, A. J., et al. Estimating the cost-effectiveness of vaccination against herpes zoster in England and Wales. Vaccine 27.9 (2009): 1454-1467.
[11] Joint Committee on Vaccination and Immunisation
Statement on varicella and herpes zoster vaccines (UK National Archives)
[12] Belongia, E. A., & Naleway, A. L. (2003). Smallpox Vaccine: The Good, the Bad, and the Ugly. Clinical Medicine and Research, 1(2), 87–92.
[13] Barquet, N., & Domingo, P. (1997). Smallpox: the triumph over the most terrible of the ministers of death. Annals of internal medicine, 127(8_Part_1), 635-642.
[14] Hoffman, H. J., Hunter, J. C., Damus, K., Pakter, J., Peterson, D. R., van Belle, G., & Hasselmeyer, E. G. (1987). Diphtheria-tetanus-pertussis immunization and sudden infant death: results of the National Institute of Child Health and Human Development Cooperative Epidemiological Study of Sudden Infant Death Syndrome risk factors. Pediatrics, 79(4), 598-611.
[15] Task Force on Sudden Infant Death Syndrome. (2005). The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics, 116(5), 1245-1255.
[16] Minor, P. D., Will, R. G., & Salisbury, D. (2000). Vaccines and variant CJD. Vaccine, 19(4), 409-410.
[17] Taylor, L,E., Swerdfeger, A,L., Eslick, G,D., (2014) Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies Vaccine 32(29):3623-3629 DOI: 10.1016/j.vaccine.2014.04.085
[18] Madsen, K,M., et al., (2002) A Population-Based Study of Measles, Mumps, and Rubella Vaccination and Autism New England Journal of Medicine 347(19):1477-1482 DOI: 10.1056/NEJMoa021134
[19] Immunization Safety Review Committee. (2004). Immunization safety review: vaccines and autism. National Academies Press.
[20] Schechter, R., Grether, J,K., (2008) Continuing Increases in Autism Reported to California's Developmental Services System Archives of General Psychiatry 65(1):19- DOI: 10.1001/archgenpsychiatry.2007.1
[21] Hviid, A., (2003) Association Between Thimerosal-Containing Vaccine and Autism JAMA 290(13):1763- DOI: 10.1001/jama.290.13.1763
[22] Ball, L. K., Ball, R., & Pratt, R. D. (2001). An assessment of thimerosal use in childhood vaccines. Pediatrics, 107(5), 1147-1154.
[23] American Academy of Pediatrics. (1999). Joint Statement of the American Academy of Pediatrics (AAP) and the United States Public Health Services (USPHS). Pediatrics, 104(3 pt 1), 568-569.
[24] Conlon A, Ashur C, Washer L, Eagle KA, Bowman MAH. Impact of the influenza vaccine on COVID-19 infection rates and severity. Am. J. Infect. Control. 2021;0(0). doi: 10.1016/j.ajic.2021.02.012.
[25] Saramago M, Bárria C, Costa VG, et al. New targets for drug design: Importance of nsp14/nsp10 complex formation for the 3’-5’ exoribonucleolytic activity on SARS-CoV-2. FEBS J. 2021. doi: 10.1111/febs.15815.
Recent vaccines News
Get customised news updates on your homepage by subscribing to articles